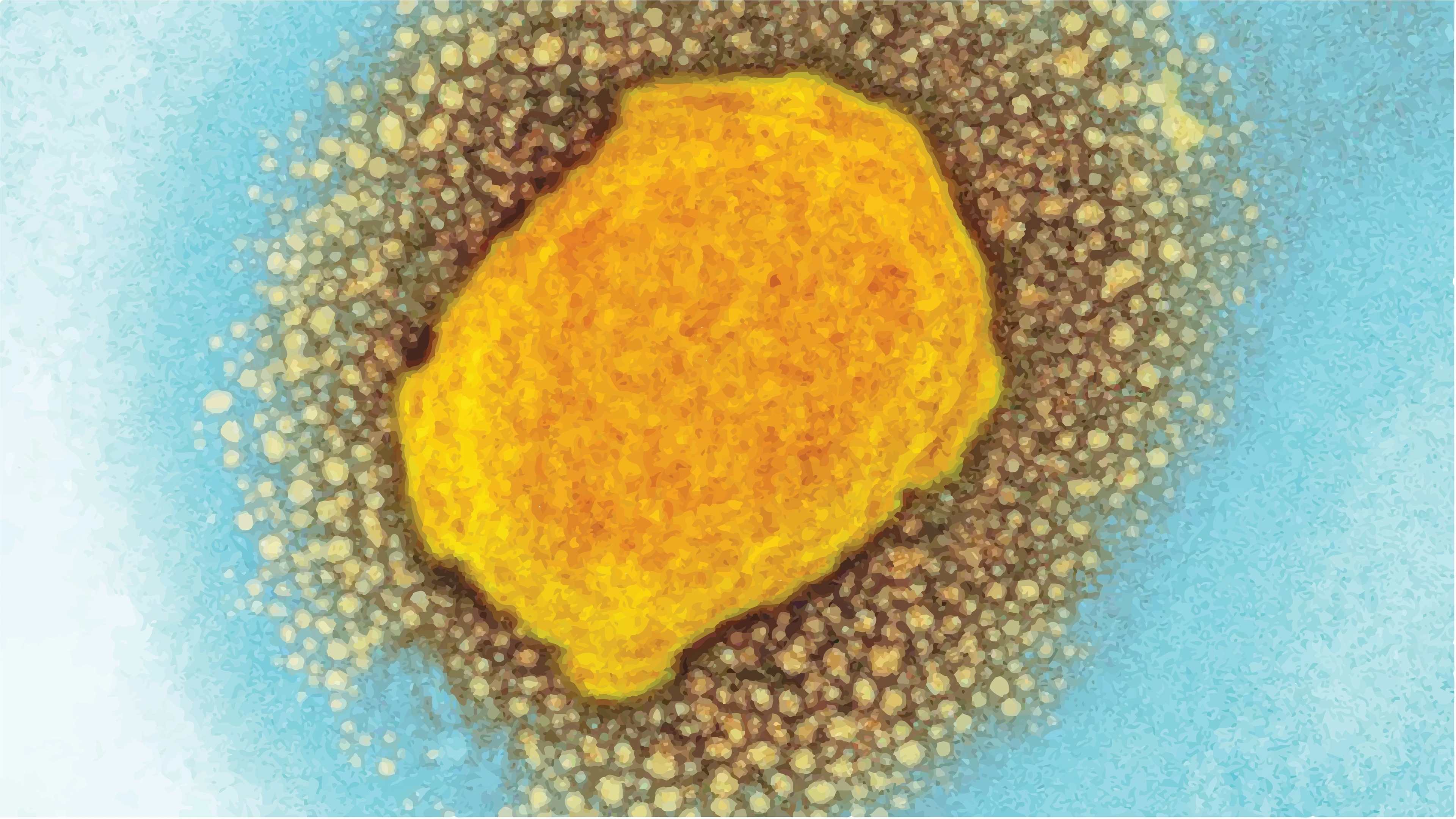
The outbreak of Monkeypox now affecting North America, Europe, and South America shouldn't come as a surprise. Outbreaks of monkeypox have been reported in Democratic Republic of Congo and other countries in West and Central Africa for decades and scientists have longed warned about the outbreak potential of this virus.
Our globally connected world has made us vulnerable to the rapid spread of new zoonoses (ie, diseases that can be transmitted to humans from animals) and the emergence of another epidemic or pandemic disease is just a matter of time. Rapid urbanisation, deforestation, intensive agriculture, livestock rearing practices, and globalisation are increasing opportunities for animal-to-human contacts and for human-to-human transmission of disease on a global scale.
However, the world is in a much stronger position to respond to and contain outbreaks of monkeypox virus in large part because of substantial and sustained investment in R&D against smallpox, a pathogen closely related to monkeypox.
Eradicating smallpox has given us the means to fight monkeypox
Smallpox, one of the deadliest diseases known to humanity, was eradicated in 1980. Smallpox plagued humankind for millennia, killing half a billion people in the 20th century alone. Its eradication was a crowning achievement of modern medicine and it is, to this day, the only human disease to be wiped from the face of the Earth.
But the eradication of smallpox wasn't the end of the story. The classification of the smallpox virus as a potential bioterrorism threat led to stockpiling of millions of doses of smallpox vaccine around the world. A global stockpile of smallpox vaccines was created, with donations from WHO member states for use in emergency responses, and this stockpile is managed by WHO. Other countries have also established their own stores of medical countermeasures against smallpox, including vaccines and antiviral drugs, in case of an outbreak or bioterrorist attack.
Decades of investments and collaborations into advanced R&D against smallpox have had a positive dual effect: they have led to the development of multiple vaccines and treatments that are effective not only against smallpox but also against other orthopoxviruses, including monkeypox.
COVID-19, and now monkeypox, have made us all too aware of an unfortunate biological truth: viruses do not respect borders. But if governments and industry can work together, transcending those same borders that viruses so effortlessly pass through, we can create a vaccine library with prototype vaccines against almost any viral threat.
Universal orthopoxvirus vaccines
The story of smallpox is a prime example of how continued and concerted commitment to vaccine R&D can strengthen the health and security of nations, while bolstering global epidemic and pandemic preparedness and response.
The R&D that underpinned vaccine development against smallpox illustrates one of the first applications of a "prototypic-vaccine approach" against pathogens from an entire genus of viruses. CEPI believes this approach should be taken a step further and applied to the 25 or so viral families known to infect humans.
The response to smallpox proves that it is possible to develop vaccines against viral threats that harbour the worst traits of a viral genus or family and thereby get a significant head start on protecting against other related threats (in fact, the smallpox vaccine as a prototype vaccine gives more than a head start; it also provides protection against all other known orthopoxviruses, including monkeypox).
In response to the current COVID-19 pandemic, CEPI is adopting a similar approach in attempting to develop broadly protective vaccines against betacoronavirus, the genus of viruses that include SARS-CoV-1, SARS-CoV-2, and MERS-CoV.
In a bid to move the world beyond a "one variant, one vaccine" approach, CEPI is supporting multiple programmes to develop a vaccine that would provide broad protection against SARS-CoV-2 variants and, in the longer term, an all-in-one betacoronavirus shot. In March 2021, CEPI's launched a $200m funding call to support development of these vaccines: nine projects are underway with more expected to be launched in the near future.
Vaccine libraries needed to defend against Disease X
Orthopoxvirus and betacoronavirus vaccines would form an important component of CEPI's planned ‘library' of vaccine candidates—a core part of its $3.5 billion pandemic preparedness plan—which are ready to be pulled off the shelf and—if needed—swiftly adapted next time an unknown pathogen (also referred to as Disease X) emerges. By having such a library at our disposal, the world wouldn't lose valuable time creating a new vaccine from scratch when a new viral threat is already upon us.
Speed is crucial when it comes to outbreak response. Vaccines can effectively control viral outbreaks and head-off a pandemic threat, but only if they are rapidly available to those who need them most, regardless of where they live. Therefore, the establishment of a global vaccine library with prototype vaccines from all relevant families will be a critical enabler of CEPI's mission to help the world compress vaccine development to 100 days.
At CEPI, we're prioritising the development of vaccine libraries for up to 10 virus families that pose the greatest risk to public health. For each virus family selected, we'll create vaccine candidates for as many as 10 to 15 different viruses depending on the complexity of the family. Our aim is to establish clinical proof of concept for vaccine libraries against multiple virus families over the next five years.
COVID-19, and now monkeypox, have made us all too aware of an unfortunate biological truth: viruses do not respect borders. But if governments and industry can work together, transcending those same borders that viruses so effortlessly pass through, we can create a vaccine library with prototype vaccines against almost any viral threat. If the global R&D community can pull off this ambitious feat, it is reasonable to foresee a future in which pandemics no longer threaten our way of life.
Learn more about CEPI's $3.5 billion pandemic plan here.


.webp)