Ebola in DRC, MERS in Saudi Arabia
Information available within this Disease Outbreak Update is produced by Program for Monitoring Emerging Diseases (ProMED).
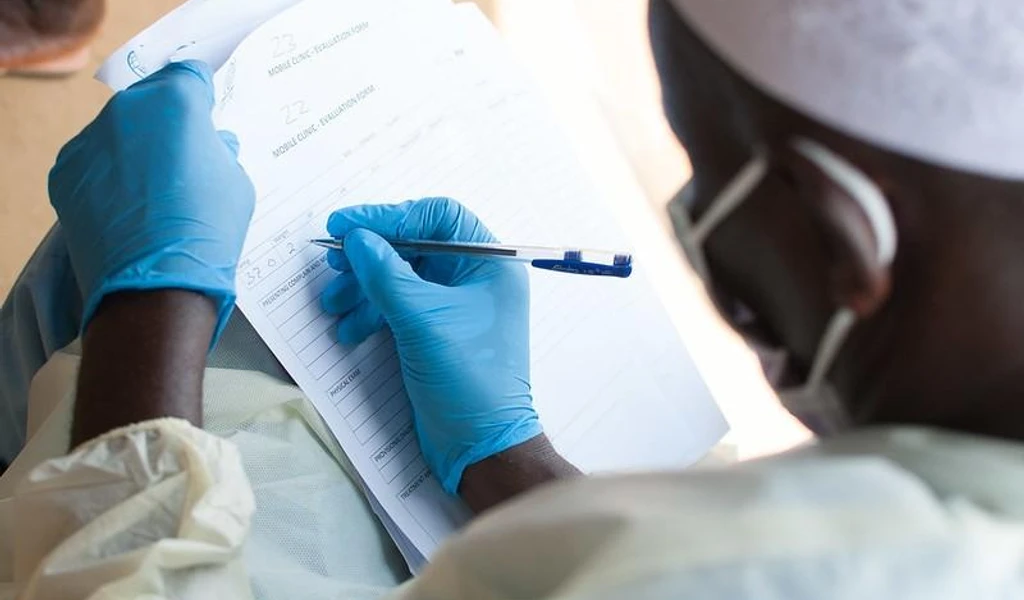
Ebola
Location
Democratic Republic of Congo (North Kivu and Ituri provinces)
Outbreak Update
Epidemiological situation report, DRC Ministry of Health, 15 May 2019
The epidemiological situation of the Ebola Virus Disease dated 14 May 2019:
Since the beginning of the epidemic, the cumulative number of cases is 1739, of which 1651 are confirmed and 88 are probable. In total, there were 1147 deaths (1059 confirmed and 88 probable) and 459 people cured.
332 suspected cases under investigation;
19 new confirmed cases, including 7 in Mabalako, 4 in Musienene, 3 in Katwa, 2 in Beni, 1 in Mandima, 1 in Lubero and 1 in Butembo;
11 new confirmed case deaths, including 6 community deaths, 2 in Mabalako, 2 in Katwa, 1 in Musienene and 1 in Butembo; 5 deaths at CTE, 2 in Butembo, 2 in Beni and 1 in Mandima.
Release of a new miraculous baby from Katwa CTE (See here)
A 42-day old baby was discharged from the Katwa CTE on Sat 11 May 2019. [D] was admitted to the CTE with her mother on 11 Apr 2019 when she was only 12 days old. Her mother, who arrived in a state of advanced coma, died at CTE the next day. D was collected on 12 Apr 2019 and was positive. After 30 days of treatment with mAb 114, D was cured. She survived thanks to the work of the health staff and the nannies who took turns at her bedside 24 hours a day but also because she was taken care of as soon as she became ill. Nannies are men and women cured of Ebola, and, therefore, immune to the virus, who care for sick children and babies during their hospitalization.
Outbreak Response
Vaccination
116 233 vaccinated persons
844 people vaccinated on the 14 May 2019.
Of those vaccinated, 31 390 are high-risk contacts (CHR), 56 334 are contacts of contacts (CC), and 28 509 are front-line providers (PPL).
Persons vaccinated by health zone: 31 283 in Katwa, 24 234 in Beni, 14 336 in Butembo, 8055.
Control Points
57 892 792 controlled people:
80 entry points (PoE) and operational health checkpoints (PoC).
As of 14 May 2019, 247 170 travelers passed control points and entry points, of which 865 (0.4%) refused screening (temperature rise) and 689 (0.3%) refused the screening (hand washing).
Funding
On Sunday 13 May 2019, the EU announced that they were ‘stepping up humanitarian support with an additional Euro 5 million [USD 5.6 million]'. With this funding, total EU funding to tackle the disease in the country amounts to Euro 17 million [USD 19 million] since 2018. See more here.
See the full ProMED post here.
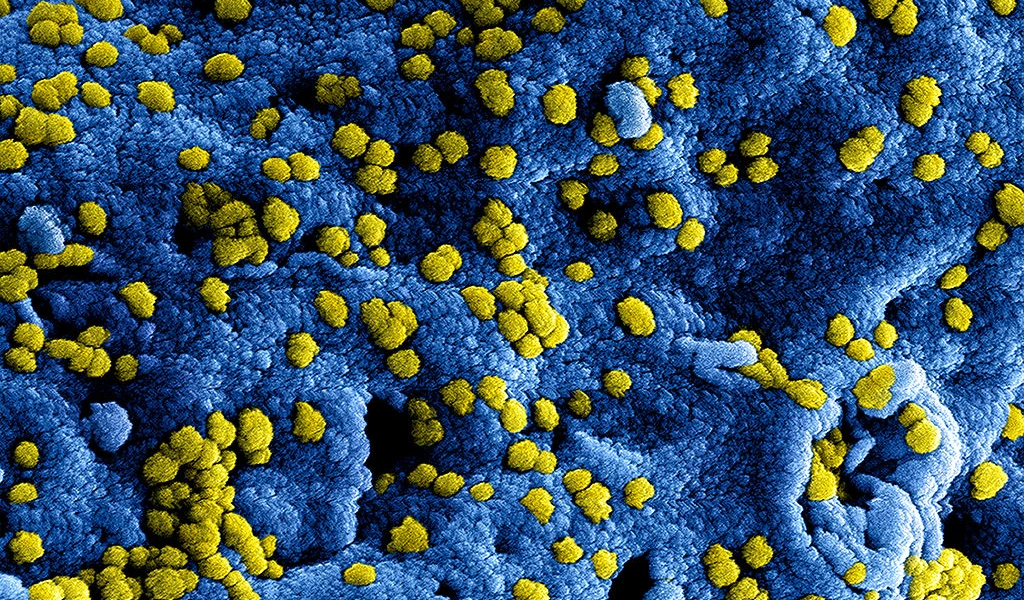
MERS-CoV
Location
Saudi Arabia
Outbreak Update
Saudi MOH 15-18 May 2019, 15-18 May 2019
In the 4 days since the last update (see MERS-CoV (47): Saudi Arabia (RI, MK) EMRO April SitRep 20190514.6469379), there has been 1 newly confirmed case of MERS-CoV infection from Saudi Arabia and 1 recovery of a previously confirmed case.
Date of confirmation report: 17 May 2019
Case no.: 19-1917
MERS from Riyadh city: 59-year-old male from Riyadh city, Riyadh region
Contact with camels: no
Case classification: primary
Current status: active
Information on newly reported recovery (1)
Case no.: 19-1909. Date of confirmation report: 19 Apr 2019. A 51-year-old male from Riyadh city, Riyadh region. Classified as a primary case, camel contact history unknown. Date of outcome report: 16 May 2019. Outcome: recovered.
WHO, Emergencies preparedness, response, Disease Outbreak News, Friday 17 May 2019
From [9 through 30 Apr 2019], the National International Health Regulations (IHR) Focal Point of Saudi Arabia reported 9 additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including 3 deaths. Of the 9 cases reported, 5 were associated with ongoing clusters in 3 cities: 3 cases (including 1 death) in Alkhafji city in the Eastern region of Saudi Arabia, 1 case in Alderb city in Jazan region, and 1 case in Alkharji city in Riyadh region of Saudi Arabia.
From 2012 through 30 April 2019, a total of 2428 laboratory-confirmed cases of MERS-CoV infection and 839 associated deaths were reported globally to WHO under the IHR. The associated deaths reported to WHO were identified through follow-up with affected member states.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high morbidity and mortality. Humans are infected with MERS-CoV from direct or indirect contact with infected dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans, especially from close, unprotected contact with infected patients. So far, the observed non-sustained human-to-human transmission has occurred mainly in healthcare settings.
Outbreak Response
WHO advice (from WHO, Emergencies preparedness, response, Disease Outbreak News, Friday 17 May 2019)
Based on the current situation and available information, WHO encourages all member states to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control (IPC) measures are critical to prevent the possible spread of MERS-CoV in healthcare facilities. It is not always possible to identify patients with MERS-CoV infection early because, as with other respiratory infections, the early symptoms of MERS are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection. Contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS. Airborne precautions should be applied when performing aerosol-generating procedures.
Early identification, case management, and isolation, together with appropriate infection prevention and control measures, can prevent human-to-human transmission of MERS-CoV.
WHO recommends that comprehensive identification, follow-up, and testing of all contacts of MERS patients be conducted, if feasible, regardless of the development of symptoms, since approximately 20% of all reported MERS cases have been reported as mild or asymptomatic. The role of asymptomatic MERS-CoV infection in transmission is not well understood. However, reports of transmission from an asymptomatic MERS patient to another individual have been documented.
MERS causes more-severe disease in people with underlying chronic medical conditions such as diabetes mellitus, renal failure, chronic lung disease, and compromised immune systems. Therefore, people with these underlying medical conditions should avoid close unprotected contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking camel's raw milk or camel urine or eating camel meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
Disease Research
An analysis of 11 MERS-CoV hospital outbreaks from 2015-2017 found substantial differences among them, highlighting complex factors that lead to case clusters.
The researchers found that the length and epidemic profiles of the outbreaks varied, some starting with a sharp rise in cases, with others beginning more slowly with isolated cases detected for a few weeks before a cluster emerged. Also, their analysis revealed that some outbreaks had a sharp decline in cases, though others had a long tail lasting several weeks after the peak.
A key public health lesson is how long it took to bring the outbreaks under control, the group wrote. All of the events reached an R0 value below 1 within 2-6 weeks after the 1st cases were identified, highlighting the timeframe in which hospital and health ministry officials can put control measures in place to stop hospital-related outbreaks.
See more in CIDRAP
The paper is also available in Nature Scientific Reports
See the full ProMED post here
Information available within this Disease Outbreak Update is produced by Program for Monitoring Emerging Diseases (ProMED).
Note: Content may be edited for style and length.