ProMED: Lassa fever monitoring across Africa and Europe after death of doctor in Sierra Leone
Epidemics can occur anywhere, at any time.
We publish regular updates, produced by Program for Monitoring Emerging Diseases (ProMED), on outbreaks of emerging infectious diseases to keep you informed on the frequency and impact of our priority diseases.
ProMED is the largest publicly-available system conducting global reporting of infectious diseases outbreaks, with ProMED staff, moderators and team members scanning for, reviewing and posting information relating to global health security from official health reports and media articles.
The below post contains information from health reports, news articles, and academic papers relating to our priority diseases, compiled together by ProMED. Content below may be edited from original ProMED posts for style and length.
These posts provide an overview of disease outbreak activity over the past several weeks. For the latest information relating to outbreaks of infectious diseases, please visit the ProMED website.
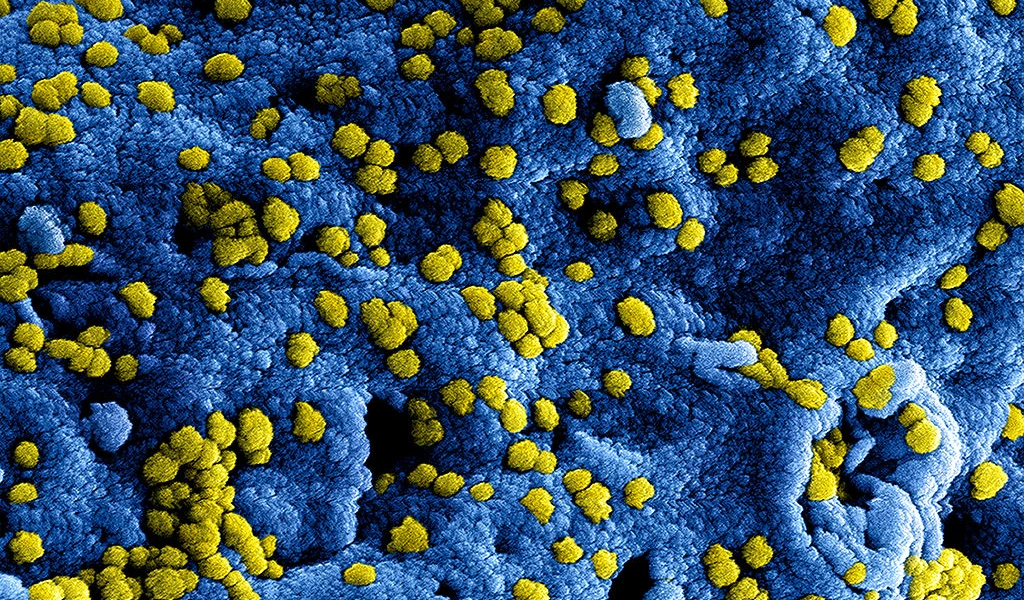
Lassa fever
Location
Sierra Leone
Outbreak Update
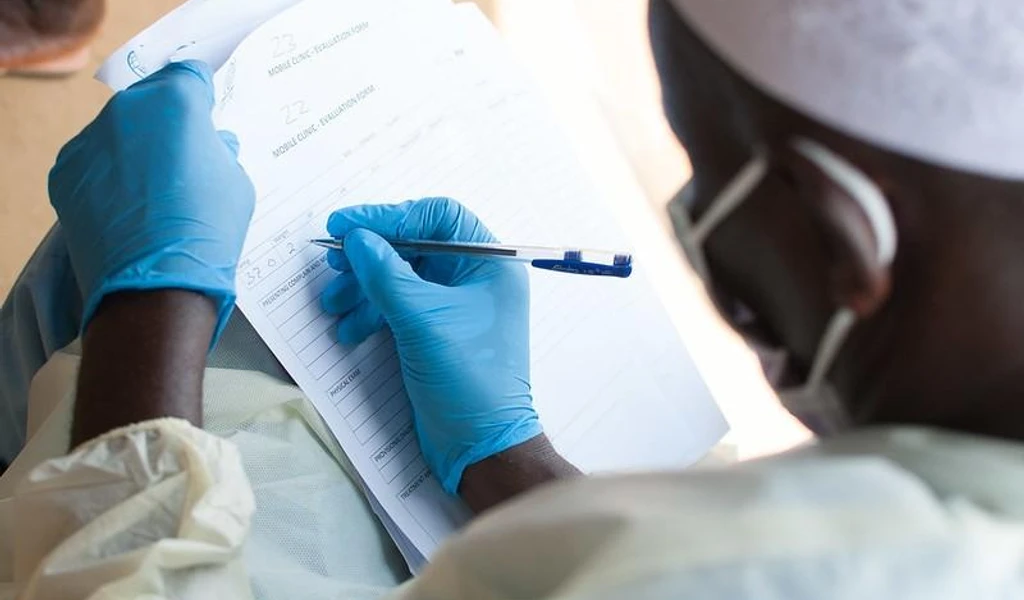
Sierra Leone health officials are working with partners at the World Health Organization and US Centers for Disease Control and Prevention and others, after a doctor from the Netherlands died of Lassa fever after likely infection from a probable patient during a surgical procedure in Masanga Hospital, where he worked.
The doctor's symptoms started a week after performing the surgery (on 11 November 2019) and included malaise and headache, followed by fever, diarrhoea, vomiting and cough. While symptomatic, he attended surgical training in Freetown, Sierra Leone on 11-12 November, where several international participants from the Netherlands and United Kingdom, in addition to 35 local participants. On 19 November, the patient was taken to the Netherlands.
Laboratory specimens from the patient tested positive for Lassa fever by polymerase chain reaction (PCR) and sequencing at Erasmus University Medical Centre in Rotterdam on 20 Nov 2019. He later died on the night of 23 November 2019.
On 22 Nov 2019, WHO was informed of a 2nd laboratory-confirmed case of Lassa fever in another Dutch healthcare worker, who also worked in the Masanga hospital. This case was subsequently medically evacuated in high containment isolation to the Netherlands and is currently under treatment. Isolation precautions have been implemented.
Contact tracing and monitoring activities have been initiated in these countries as required:
Sierra Leone
As of 24 November 2019, in addition to the 2 Dutch cases, 2 further cases among national healthcare workers, one confirmed and another suspected, have been reported from Masanga hospital. Both healthcare workers were involved in the management of the 2 surgical patients operated by the Dutch doctor. All high-risk contacts in Masanga hospital are being monitored.
The Netherlands
Several high- and low-risk contacts have been identified among personal contacts and healthcare workers. According to Dutch protocols, they will be monitored until 21 days after the last potential exposure. Five high-risk Dutch contacts who were in Sierra Leone have been repatriated through a dedicated flight and are now under monitoring.
Germany
The 4 medical evacuation flight staff (2 pilots and 2 healthcare workers) spent 8 flight hours in a confined space in the ambulance plane without any barrier between the cockpit and cabin. They have been assessed as moderate-risk contacts. According to German recommendations, they are being monitored for 21 days following the last potential exposure.
United Kingdom (UK)
UK authorities have identified 18 UK nationals as contacts of the 1st Dutch case. Of these 18, 8 are high-risk contacts and were exposed in Masanga hospital while working alongside the doctor or may have been exposed to the 2 patients he operated on. Of these 8 high-risk contacts, 7 returned to the UK and one went to Uganda. In addition, 13 UK nationals attended the surgical training event in Freetown, Sierra Leone. Of these 13 participants, 3 came from Masanga hospital and belong to the above group of 8 high-risk contacts. The remaining 10 participants were possibly exposed during the training and are considered low-risk contacts. Of these 18 contacts identified, 17 have returned to the UK and are under public health follow-up for 21 days; one high-risk contact went to Uganda. UK authorities are in contact with the organizers, and the names of participants from Sierra Leone and the Netherlands have been shared with respective National IHR Focal Points.
Uganda
One contact, a UK national, who may have been exposed in Masanga hospital subsequently travelled to Uganda. They are now being followed up by the Uganda authorities, and the UK authorities are providing support remotely though public health and consular channels.
The National IHR Focal Point of the Netherlands has also informed their counterpart in Morocco about the potential risk of exposure at the Agadir Airport. Morocco National IHR Focal Point confirmed that the investigation is conducted, and control measures have been implemented to ensure there was no transmission in Agadir.
Sierra Leone is endemic for Lassa fever. Previously, sporadic cases have been exported to Europe from endemic countries in Africa, such as Togo, Liberia and Nigeria. In 2018, a total of 23 confirmed Lassa fever cases with 14 deaths (case fatality rate 61%) were reported from 2 districts of Sierra Leone: Bo district (2 cases; 2 deaths) and Kenema district (21 cases; 12 deaths).
From 1 Jan-17 Nov 2019, of the 182 suspected cases, 10 cases with 6 deaths (case fatality ratio 60%) have been confirmed for Lassa virus infection. All confirmed cases during this period were reported from Kenema district, which has been reporting cases of Lassa fever every year.
WHO continues to advise all countries in the Lassa fever belt due to the need to enhance early detection and treatment of cases to reduce the case fatality rate as well as strengthen cross-border collaboration. WHO advises against any restrictions on travel or trade to or from Sierra Leone based on the current available information.
Sources:
WHO — Lassa fever — The Netherlands (ex — Sierra Leone), 28 November 2019
See the full ProMED post
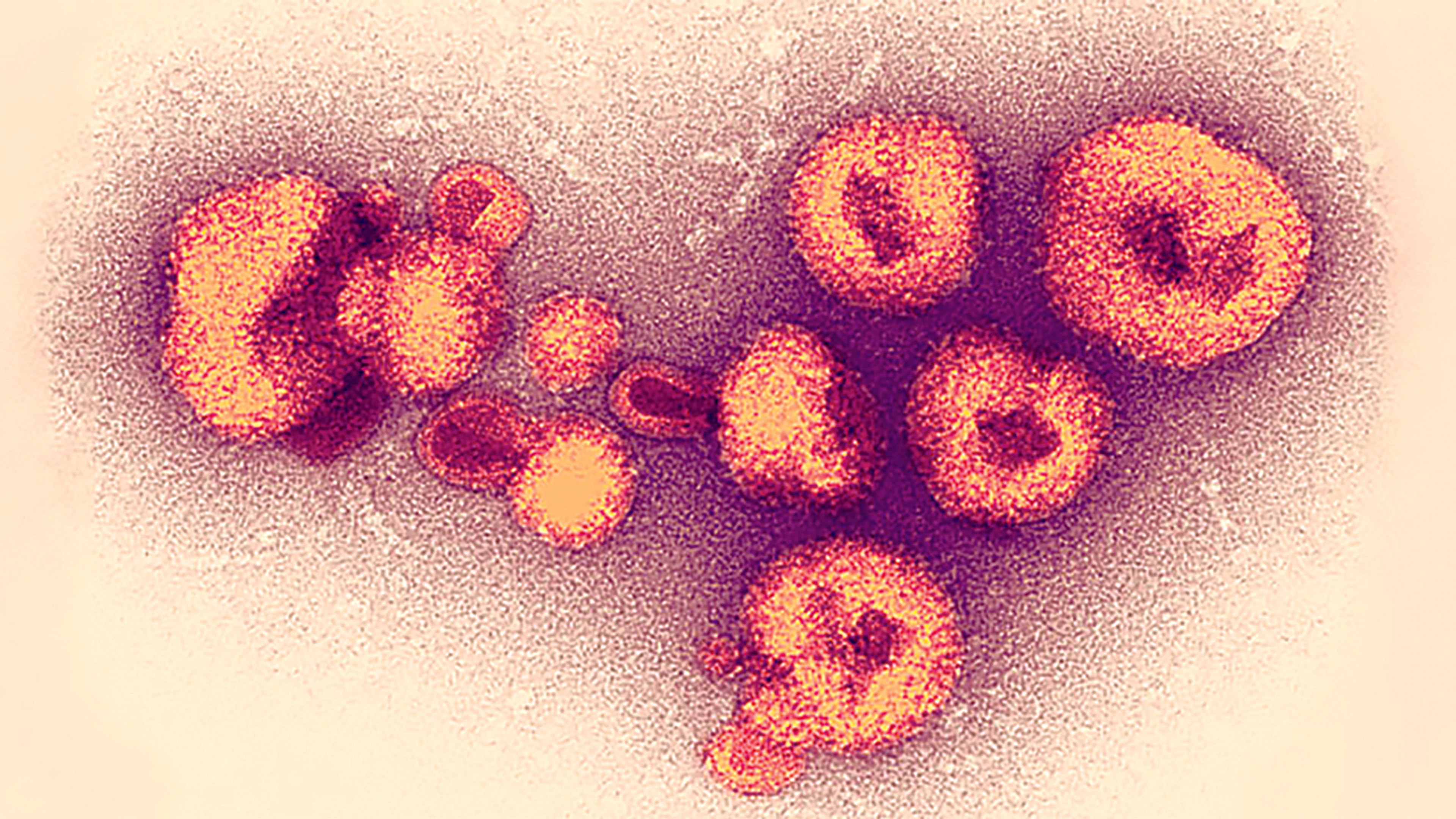
Ebola
Location
Democratic Republic of Congo
Outbreak Update
As of 25 November 2019, the cumulative number of cases is 3304, of which 3186 are confirmed and 118 are probable. In total, there were 2199 deaths (2081 confirmed and 118 probable) and 1077 people healed.
- 392 suspected cases under investigation;
- 1 new case confirmed in North Kivu in Mabalako;
- no new deaths among confirmed cases;
- no cured persons have been released from Ebola treatment centres [ETCs];
- no health worker is among the new confirmed cases. The cumulative number of confirmed/probable cases among health workers is 163 (5% of all confirmed/probable cases), including 41 deaths.
To date, 255 215 people have been vaccinated with rVSV-ZEBOV vaccine, produced by Merck, and 724 have been vaccinated with the second Ebola vaccine, produced by Johnson and Johnson.
Since the beginning of the epidemic, the total number of travelers checked (temperature measurement) at the sanitary control points is 120 825 670.
On 26 November, the World Health Organization (WHO) and the UN Children's Fund (UNICEF) evacuated dozens of their staff working on the Ebola epidemic from the town of Beni in DRC due to the worsening security situation.
Disease Research Updates
On 27 November 2019, an international research group, which includes renowned Ebola researcher and DRC health official Jean-Jacques Muyembe Tamfum, published its full results from a clinical trial of 4 Ebola therapies used in the DRC outbreak, in the New England Journal of Medicine.
In August [2019], an independent board that was monitoring the study in people treated in DRC Ebola treatment units took an early look at the data and saw that mortality rates were significantly lower in those who received the monoclonal antibody cocktail REGN-EB3 (made by Regeneron of Tarrytown, New York) and the single monoclonal antibody mAb 114, developed from antibodies of an Ebola survivor.
The other 2 therapies in the trial were the triple monoclonal antibody ZMapp, used as a control, and the antiviral drug remdesivir.
Patients in the study were randomized to receive one of the drugs, plus standard care. The trial began in November 2018 and enrolled 681 patients. To compare the 4 treatments, the researchers assessed their impact against death at 28 days.
Mortality was lower in the mAb114 group, 35.1%, compared with 49.7% in those who got ZMapp. For REGN-EB3, mortality was 33.5%, compared with 51.3% in a ZMapp subgroup. And for remdesivir, overall mortality was 53.1%. Results were even more impressive for patients who had low viral loads. The team identified four serious adverse events that were possibly related to the trial drugs.
The group concluded that both mAB114 and REGN-EB3 are superior to ZMapp in reducing death from Ebola and that it's possible to conduct ethically sound clinical research in an outbreak setting.
Sources:
DRC CMRE Team - Daily Epidemiological Situation Update (translated from French), 26 November 2019
New England Journal of Medicine — A Randomized, Controlled Trial of Ebola Virus Disease Therapeutics
CIDRAP — New data highlight promise of 2 Ebola treatments, 27 November 2019
See the full ProMED post
MERS
Location
Saudi Arabia
Outbreak Update
Since the last update by the Saudi Arabia Ministry of Health on 13 November 2019, there have been a total of 3 newly confirmed cases of MERS-CoV infection reported in the country, with 11 newly reported outcomes (2 deaths and 9 recoveries).
During the month of November 2019, there were a total of 12 newly confirmed cases of MERS-CoV infection reported by Saudi Arabia, including one death. Cases were reported from 4 different regions: Riyadh (7), Al Madinah (2), Makkah (2) and Al Qasim (1). Classifications of cases included one secondary case, and 11 primary cases, of whom 5 were reported to have had known camel contact preceding onset of illness.
Sources:
Saudi Arabia Ministry of Health — 14 November to 1 December 2019