Recently, I had the chance to speak about how central equitable access is to the success of CEPI's overall mission at the 2019 World Conference on Access to Medical Products Achieving the SDGs 2030.
Indeed, as Richard Hatchett, CEPI's Chief Executive, highlighted earlier this year "you can't beat epidemics without equitable access to vaccines".
CEPI is 100% committed to achieving equitable access to all of our vaccines. This commitment drives every aspect of our work and is key to our success as a global health organisation.
But what do we actually mean when we're talking about equitable access to these vaccines?
Equitable access in the context of an outbreak
When it comes to CEPI's vaccines, equitable access in the context of an outbreak means that appropriate vaccines are first available to populations when and where they are needed to end an outbreak or curtail an epidemic, regardless of ability to pay. This core principle underpins all of our work.
Access to the data, research results, and publications resulting from CEPI-funded vaccine development is also crucial. As is ensuring access to biological materials that can help to accelerate vaccine development. Enabling access to this kind of information will help to streamline vaccine development by improving the collective knowledge base of our partners, reducing the chance of duplicating research, and enhancing research collaboration.
CEPI's approach to equitable access
Developing a single vaccine product can take years, requiring a huge collective effort on the part of vaccine developers, regulators, and healthcare systems. So developing and ensuring equitable access to the 26 vaccine candidates that CEPI currently has in its vaccine portfolio is no mean feat.
Each of our vaccine candidates is designed to address a specific problem, which can affect a specific population, living in a specific environment. Therefore, a blanket "Equitable Access Policy" can never anticipate all of the detailed access needs associated with our diverse and ever-growing vaccine portfolio.
CEPI weaves the principle of equitable access into every aspect of vaccine development, from the micro level to the macro level.
Let's look at the micro-level. We might have a vaccine candidate, for example, that is safe. But what if it had to be transported at —80 degrees centigrade to remain effective? And what if manufacturing processes were so complex that it can only be manufactured in an expensive facility in the Northern Hemisphere? In this scenario, the vaccine candidate would almost certainly be unsuited for use against an emerging infectious disease in a low-income country with a weak healthcare system. To avoid such a scenario CEPI works with partners, right from the start of the vaccine-development process, to ensure that the technical aspects of vaccine development are specifically designed to ensure that they are accessible to populations in territories affected by the diseases we are working on.
On the other end of the spectrum, a vaccine candidate might be ready for large-scale testing in an outbreak situation, but if healthcare authorities in affected countries are not set up to deploy one of our vaccines, then CEPI won't be able to get its vaccines to the people who need them in time to end an outbreak or curtail an epidemic. Therefore, CEPI works with manufacturers and regulatory partners to prepare for possible emergency use, to consider alternate regulatory pathways, and facilitate decisions on regulatory approvals and launch. CEPI is committed to working with countries at risk and other implementation partners to anticipate and overcome operational barriers to rapid deployment and use of our vaccine candidates.
Working together to achieve Equitable Access
CEPI is nearing its third year of existence. In this short period of time, we've committed up to $456 million in vaccine development. This investment includes 26 vaccine candidates against six of the eight categories of emerging infectious diseases that the WHO has said need urgent R&D funding.
Our progress has been swift, and our equitable access policy has had to adapt just as fast. We have published our Equitable Access Policy, we've published a paper that explains how our equitable access policy is being implemented, and we've published a roadmap of how equitable access will be secured in future partnering agreements. We have also built equitable access considerations into the way we work—through our management of projects at stage-gate reviews (during which important go-no-go points in our projects are assessed) and by incorporating equitable access into our integrated product development plans. CEPI has also just established an Equitable Access Committee of the CEPI Board to provide strategic oversight of our approach to equitable access.
As the scientific, political, and global health challenges we face continue to evolve, so too must our approach to implementing our equitable access policy. But the core principle is immutable—in an outbreak, CEPI is charged to ensure that appropriate vaccines are first available to populations when and where they are needed to end an outbreak or curtail an epidemic, regardless of ability to pay. Failure is not an option. That's why CEPI will work tirelessly with our partners to address key access issues—like development of investigational stockpiles of vaccines for emergency use, access to intellectual property, access to R&D data and materials, and pricing upon licensure of a vaccine.
As a global coalition of public-sector, private-sector, and civil society partners, from which we draw significant support, I believe CEPI is uniquely placed to rise to this challenge.
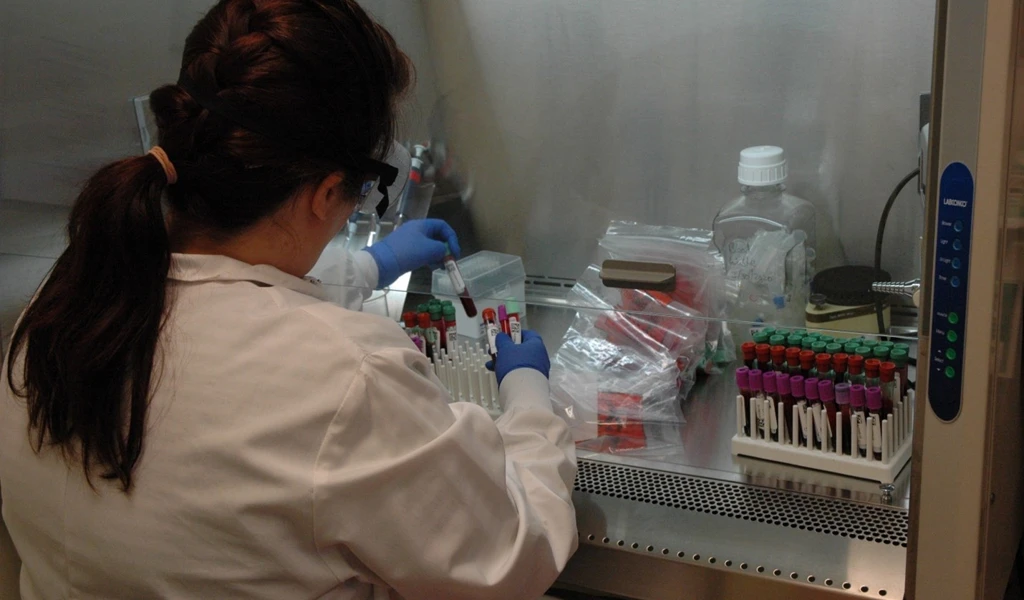
Image credit: UNMEER/Aalok Kanani